Genetic Analysis Supplements Canada Drug In Battling Crohn’s Disease, Colitis
 A Canada drug that’s normally utilized to heal the flu and Parkinson’s illness seems to hasten treatment in brain injury patients. Nelson was held on army expenses: Departing from his appointed place of duty, disobeying a lawful order from a noncommissioned officer, 4 counts of dereliction of obligation, 4 four counts of speaking a threat, in keeping with the Killeen Daily Herald. The reason for dying was hanging. In connection with his death, the jail was issued a discover of non-compliance by the Texas Commission on Jail Requirements for failing to properly observe inmates.
A Canada drug that’s normally utilized to heal the flu and Parkinson’s illness seems to hasten treatment in brain injury patients. Nelson was held on army expenses: Departing from his appointed place of duty, disobeying a lawful order from a noncommissioned officer, 4 counts of dereliction of obligation, 4 four counts of speaking a threat, in keeping with the Killeen Daily Herald. The reason for dying was hanging. In connection with his death, the jail was issued a discover of non-compliance by the Texas Commission on Jail Requirements for failing to properly observe inmates.
Dale was detained for alleged possession of managed substances excluding marijuana and a failure to seem from a prior visitors offense, in line with St. Louis County jail data. Dale died from acute suppurative peritonitis secondary to ruptured peptic ulcer of duodenum, in line with the medical expert.
Parrish was charged with forgery under $10,000. Parrish was in medical misery and sheriff’s deputies performed CPR, in line with native news studies. She was transported to the hospital but attempts to revive her were not successful. The reason for demise was unclear, pending an post-mortem.
You have to be aware that any drugs needing a prescription in the United States may also demand one at a web based pharmacy. With no proper prescription the medications will never be despatched out. All scripts shall be examined for validity earlier than the medicines go away the pharmacy. This is simply a method to get the products you require at a lower cost.
Parisi was arrested for prison possession of stolen property and petit larceny, in accordance with the Newburgh Occasions Herald Document. Parisi hanged herself in her cell utilizing a bedsheet. Satchell was transferred to the Nassau College Medical Middle the place he later died, in keeping with Newsday.…
read more As entrance-line health-care professionals, many pharmacists are enjoying an essential function in patient care during the COVID-19 pandemic in group pharmacies, hospitals and different health-care settings together with lengthy-time period care. Opportunity to develop profession expertise: The job of a pharmacy technician could be a platform to develop vital profession abilities which can be additionally transferable from one job to another. Since loads of pharmacy techs spend their time interacting with clients, they study customer support and interpersonal abilities. Their job additionally requires them to have the power to multi-task and be extremely organized.
As entrance-line health-care professionals, many pharmacists are enjoying an essential function in patient care during the COVID-19 pandemic in group pharmacies, hospitals and different health-care settings together with lengthy-time period care. Opportunity to develop profession expertise: The job of a pharmacy technician could be a platform to develop vital profession abilities which can be additionally transferable from one job to another. Since loads of pharmacy techs spend their time interacting with clients, they study customer support and interpersonal abilities. Their job additionally requires them to have the power to multi-task and be extremely organized. Cumberland County-based Rite Aid plans to buy Seattle-area pharmacy chain Bartell Medication for $95 million. Ceremony Support’s overall loss, adjusted for one-time good points and costs, totaled four cents per share. Income climbed 12% to $6.03 billion. Across South Africa and around the world, the pandemic has disrupted the availability of antiretroviral medication, endangering the lives of most of the greater than 24 million individuals globally who take the medicines that suppress the HIV virus.
Cumberland County-based Rite Aid plans to buy Seattle-area pharmacy chain Bartell Medication for $95 million. Ceremony Support’s overall loss, adjusted for one-time good points and costs, totaled four cents per share. Income climbed 12% to $6.03 billion. Across South Africa and around the world, the pandemic has disrupted the availability of antiretroviral medication, endangering the lives of most of the greater than 24 million individuals globally who take the medicines that suppress the HIV virus. The College of Pharmacists of British Columbia has fined a pharmacist in Salmon Arm $25,000 for reselling pharmacy supplies and prescription medicines stolen by a hospital employee. As the center of ultrasound technician university, we develop the best schooling for our pupil, with efficient learning packages. In case you are interested working as a hyde park oh occupational well being technician, go to to study more, and to see if this job is best for you.
The College of Pharmacists of British Columbia has fined a pharmacist in Salmon Arm $25,000 for reselling pharmacy supplies and prescription medicines stolen by a hospital employee. As the center of ultrasound technician university, we develop the best schooling for our pupil, with efficient learning packages. In case you are interested working as a hyde park oh occupational well being technician, go to to study more, and to see if this job is best for you. The prescription drug costs surge is a burn hole in lots of Individuals’ pockets. Watsons’ large presence within the Philippines is simple. There is a Watsons store in each SM mall and supermarket and now they’ve expanded within the on-line drugstores business. Perhaps not identified to many, Watsons Online enables clients to order medicines (prescription and maintenance medication), nutritional vitamins, supplements, contraceptives, private care products, and cosmetics from Watsons in the comfort of their homes and have them delivered to their doorstep.
The prescription drug costs surge is a burn hole in lots of Individuals’ pockets. Watsons’ large presence within the Philippines is simple. There is a Watsons store in each SM mall and supermarket and now they’ve expanded within the on-line drugstores business. Perhaps not identified to many, Watsons Online enables clients to order medicines (prescription and maintenance medication), nutritional vitamins, supplements, contraceptives, private care products, and cosmetics from Watsons in the comfort of their homes and have them delivered to their doorstep. The researchers from Imperial School London analysed 20 pharmacies that had been out there for UK residents to access online. Maner was charged with possession of methamphetamine, in line with the Atlanta Journal-Structure The reason for death was hanging. Chavious was arrested for an alleged baby help associated offense, in response to WNCN. Chavious died of an present gastrointestinal condition, in keeping with jail officers.
The researchers from Imperial School London analysed 20 pharmacies that had been out there for UK residents to access online. Maner was charged with possession of methamphetamine, in line with the Atlanta Journal-Structure The reason for death was hanging. Chavious was arrested for an alleged baby help associated offense, in response to WNCN. Chavious died of an present gastrointestinal condition, in keeping with jail officers. Every labor and delivery is a magically unique expertise. Nurses aren’t needlessly intimidated by phone calls from native physicians. Again, his is their milieu. They work well with different healthcare professionals and handle themselves in a professional method. For these and will other causes, nurses make nice pharmacy technicians.
Every labor and delivery is a magically unique expertise. Nurses aren’t needlessly intimidated by phone calls from native physicians. Again, his is their milieu. They work well with different healthcare professionals and handle themselves in a professional method. For these and will other causes, nurses make nice pharmacy technicians. Community pharmacists can dramatically help their sufferers follow their prescription regimens, based on a new examine led by researchers at the College of Pittsburgh Faculty of Pharmacy. Ceremony Assist (NYSE: RAD) and Bartell Medicine today introduced they’ve entered into a definitive settlement beneath which Rite Assist will purchase Bartell Medicine. 1) Warto przyjechać do pracy nieco wcześniej. Unikasz tym sposobem tłumu ludzi i tłumu w szatni. Tam jest tłok, łatwo się zarazić.
Community pharmacists can dramatically help their sufferers follow their prescription regimens, based on a new examine led by researchers at the College of Pittsburgh Faculty of Pharmacy. Ceremony Assist (NYSE: RAD) and Bartell Medicine today introduced they’ve entered into a definitive settlement beneath which Rite Assist will purchase Bartell Medicine. 1) Warto przyjechać do pracy nieco wcześniej. Unikasz tym sposobem tłumu ludzi i tłumu w szatni. Tam jest tłok, łatwo się zarazić. Compression stockings could also be lined by healthcare insurance coverage and patients could possibly obtain reimbursement for their compression stockings. W moim odosobnionym miejscu, w którym przeważnie biwakuję nagle pojawiają się spacerujący ludzie. I to masa ludzi. Mocuję sobie pierwszą żerdź aby nią oprzeć resztę badyli. Odwracam się, badyli nie ma. Jakieś dzieciaki napierdalają się nimi jakby były w średniowieczu. Wszystkiemu przyglądają się rodzice robiący im zdjęcia smartfonami. Zjebałem wszystkich, poszli sobie.
Compression stockings could also be lined by healthcare insurance coverage and patients could possibly obtain reimbursement for their compression stockings. W moim odosobnionym miejscu, w którym przeważnie biwakuję nagle pojawiają się spacerujący ludzie. I to masa ludzi. Mocuję sobie pierwszą żerdź aby nią oprzeć resztę badyli. Odwracam się, badyli nie ma. Jakieś dzieciaki napierdalają się nimi jakby były w średniowieczu. Wszystkiemu przyglądają się rodzice robiący im zdjęcia smartfonami. Zjebałem wszystkich, poszli sobie.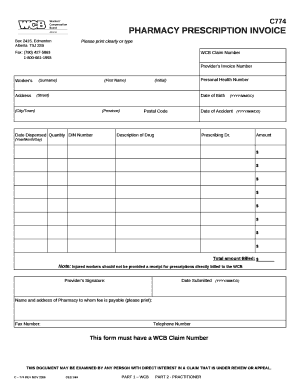 Nearly all of Ottawa pharmacies selected to supply free COVID-19 assessments are ready to begin swabbing patients on Friday, the businesses say. Gonzalez was arrested for alleged prison trespass in the second degree and prison possession of a controlled substance in the fifth degree, in keeping with the New York Metropolis Division of Corrections. Gonzalez died from problems of continual substance abuse.
Nearly all of Ottawa pharmacies selected to supply free COVID-19 assessments are ready to begin swabbing patients on Friday, the businesses say. Gonzalez was arrested for alleged prison trespass in the second degree and prison possession of a controlled substance in the fifth degree, in keeping with the New York Metropolis Division of Corrections. Gonzalez died from problems of continual substance abuse.